Care Pathways are an important tool in the translation of evidence-based medicine to the delivery of high quality, high value care. However, despite existing conceptual frameworks that define what care pathways are, an important gap remains with respect to pathway management in how managers can effectively mobilize their organizations to develop pathway programs.
To address this gap, VSSL members Christopher Chen, Leah Marcotte, and Joshua Liao, and Valley Medical Center Chief Quality Officer Kim Herner, drew upon a combination of theory and collective experience of driving value-based care delivery to describe an applied framework to support the development of pathway programs aimed at improving quality and value.

Their Approach
Defined Care Pathways as vehicles for providing evidence based care through standardized processes, supported by a program of monitoring and improvement for a defined population of patients or clinical condition
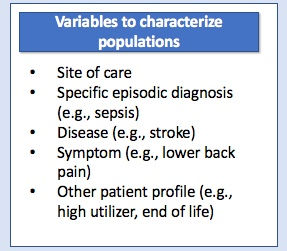
Identified the first step of the framework as defining the population, which could be done along several variables:
Identified the second step of the framework as defining the pathway program goals with respect to 4 key processes
Developing evidence-based guidelines
Operationalizing guidelines into standard processes
Monitoring pathway implementation and performance
Improving and iterating pathway components

The framework defines these processes and outlines resource allocation approaches based on institutional capability.
For example, a resource-light approach might be most appropriate for developing evidence based guidelines in a small community hospital, necessitating the usage of off-the-shelf guidelines.
A resource-intense approach might be more appropriate for a large academic medical center with the capability to review primary and secondary literature with content experts.
What It Might Look Like
Breaking Care Pathways down into specific operational components can facilitate alignment and focus when developing and implementing new programs


In the examples shown, our framework has helped achieve programmatic clarity at UW Medicine Valley Medical Center when:
Defining a pathways population: target populations for pathways were plotted along a spectrum of care settings to create a broader view of where our program staff was investing the most resources
Setting targets for individual pathway components: overlaying individual pathways such as COPD and glycemic control over the framework can help achieve direction when creating goals and allocating resources
Want to learn more? See the full-length paper by Drs. Chen, Marcotte, Herner, and Liao published in the Journal of Clinical Pathways.
.jpg)
Comments